Newcastle and Hunter-based researchers have discovered a drug combination that could improve the life expectancy of children with brain cancer, extending their average survival from 11 to 20 months.
Diffuse Midline Gliomas (DMG), including Diffuse Intrinsic Pontine Gliomas (DIPGs), are the most lethal of childhood cancers.
Published in Cancer Research, University of Newcastle, and the Hunter Medical Research Institute (HMRI) researchers have uncovered the mechanisms controlling response to the promising oral therapy ONC201, which is currently being investigated in 12 clinical trials worldwide, across many cancer types.
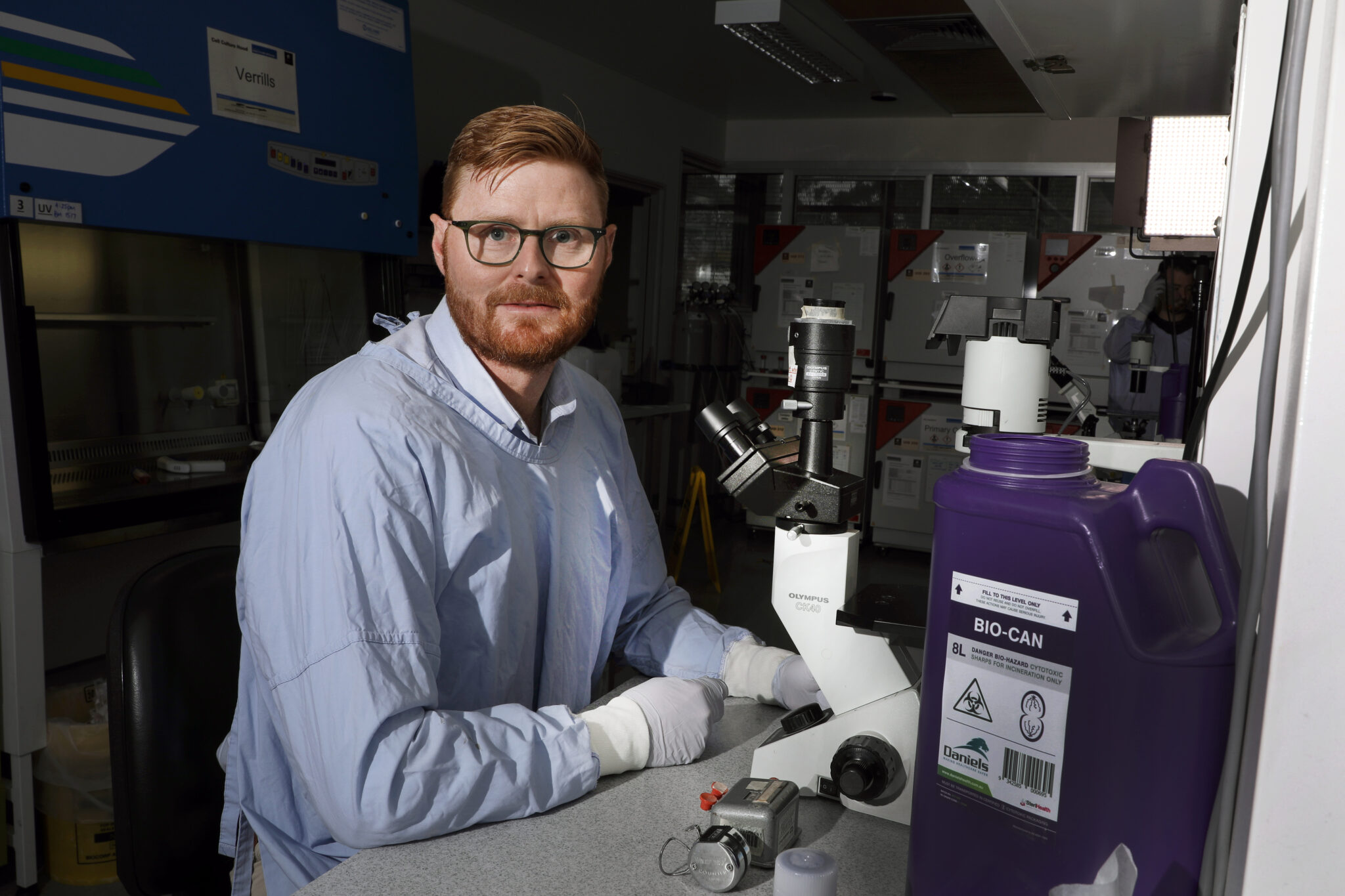
One of those trials, Combination Therapy for Diffuse Midline Glioma, (research trial known as PNOC022), was established using the preclinical data largely generated by lead investigator Professor Matt Dun and his University of Newcastle research team.
“ONC201 appears to improve some patient outcomes, extending median survival to 20, from 11 months,” Matt said.
Professor Matt Dun and his team also discovered the mechanisms controlling resistance to ONC201, and a strategy to combat this through combination with a second drug, paxalisib and standard of care treatment, radiotherapy.
Using cell lines derived from DMG patient tumour samples (each with different genetic features), the University of Newcastle’s Cancer Signalling Research Group (CSRG) assessed how each tumour type responded to the therapy ONC201.
Determining that ONC201 treatment increased the activity of the PI3K signalling pathway was surprising, particularly as Professor Dun and his team had already discovered a different drug in DMG – paxalisib, which acts on this target.
At the time, paxalisib was already in clinical trials as a single drug treatment. The team used its DMG models to test the effect of the drugs in combination, finding them beneficial and safe, progressing the strategy to clinical trial.
Matt said the oral therapy ONC201 appeared to be extending the survival of patients with DMG. The team’s research paper highlights case studies of children on the combination, some of whom have experienced a reduction in their tumour size and an extension of survival.
“As more data becomes available, we’ll know the extent of benefit,” Matt said.
“PNOC022 opened in the United States in 2021 and Australia in 2022, and is now also recruiting in New Zealand, The Netherlands, Switzerland and Israel,” he said.
Currently, approximately 100 children are receiving ONC201+paxalisib combination therapy worldwide.
Matt said their specialist techniques had revealed how two emerging therapies exerted their anti-cancer effect, particularly, the mechanisms controlling whether a patient responded, and the benefits of using them in combination.
“We are continuing to study these drugs in our lab-based DMG models so we can understand how to improve the number of people who respond, or the length/robustness of response a patient might experience, to improve survival outcomes,” Matt said.
“This involves additional supportive medicines, manipulating the dosing schedule and further investigation into how to enhance response in resistant tumours.
“Thirteen is the number of years that gets thrown around as the time it takes to move research findings from bench to bedside.
“I’d really like to highlight that our dedicated efforts have achieved this in less than five.
“This leaves families with no hope, an indispensable element when dealing with a cancer diagnosis. The path to move our findings from the lab to the clinic has happened with a number of international collaborators on board.
“It will be great to build on that spirit of collaboration in Australia so more of the great work being done locally can improve survival of kids with cancer.”